At a time when much of the news is dismaying, last week brought a development that was, for a change, truly joyous. The rescue of a Thai soccer team, along with their coach, from the cave where they had been trapped for 18 days was a welcome conclusion to an at-times harrowing tale. While the death of one of the team’s rescuers—former Thai Navy SEAL Saman Kunan—prevents this ending from being an unequivocally happy one, the fact that the team is now out of immediate physical danger is something we can all celebrate.
Yet while this danger may have passed, the rescued team still faces a potentially long road to recovery. They have suffered a trauma, and trauma can have a lingering and profound effect on physical and mental health.
Traumatic events are a near-ubiquitous human experience. A general population surveyconducted in 24 countries showed that more than 70 percent of respondents experienced a traumatic event, and 30.5 percent had experienced four or more events. Traumatic events(TEs) range from threatened death, serious injury, or sexual violence, to the unexpected death of loved ones. The most common TE exposures include the unexpected death of a loved one, mugging, experiencing a life-threatening vehicle accident, or experiencing a life-threatening illness or injury. Figure 1 indicates the prevalence of exposure to any traumatic event in the 24 countries that were included in the survey, showing substantial heterogeneity by country, with the lowest exposure in Bulgaria (28.6 percent) and the highest in Ukraine (84.6 percent). The US (82.7 percent) ranks among those countries with the highest levels of TEs.
Figure 1. Prevalence of exposure to any traumatic event in each survey of the 24 countries
Benjet C, et al. The epidemiology of traumatic event exposure worldwide: Results from the World Mental Health Survey Consortium. Psychological Medicine. 2016; 46(2): 327—343.
The Physical and Mental Health Consequences of Traumatic Events
Responses to TEs may vary individually, and include a range of health consequences from chronic inflammation to Post-Traumatic Stress Disorder (PTSD).
Starting with physical health, TEs clearly affect health as a direct result of the trauma itself, resulting in documentable injury. Effects, however, extend well beyond the TE. Well-documented physical health consequences of TEs include disruptions to cardiovascular, immune, reproductive, neuroendocrine, brain, and gastrointestinal function. For example, witnessing or experiencing a TE can cause long-term changes in systolic blood pressure and atrioventricular defects; it can also drive risk for coronary events. PTSD is associated with altered blood coagulation; this may, in part, account for the development of cardiovascular disease among patients with PTSD. Empirical evidence demonstrates that although acute stress may immediately improve immune function, chronic stress is associated with immunosuppression and greater vulnerability to disease in the longer term. One particular consequence of TEs that has been much in the press is traumatic brain injury (TBI). TBI is a common injury associated with TEs in military and civilian populations alike. TBI is the result of a blow or jolt to the head that disrupts the function of the brain. Leading causes of TBI include having a fall, being struck by an object, and being in a motor vehicle crash. The severity of TBI may range from “mild” (i.e., a brief alteration in mental status) to “severe” (i.e., an extended unconscious period following the injury). According to the CDC, TBI was associated with nearly 2.8 million emergency department visits, hospitalizations, and deaths in 2013. Among a sample of people hospitalized after a TBI, almost half (43 percent) suffered from related disabilities one year after the injury. Another study estimated that in 2005, about 1.1 percent of Americans lived with a long-term disability caused by TBI.
PTSD is the sentinel psychiatric disorder associated with traumatic events. PTSD symptoms include intrusive re-experiencing symptoms, avoidance of stimuli associated with the TE, arousal and reactivity, and disturbances in mood and cognition. In the US, the lifetime prevalence of PTSD is approximately 8 percent, with prevalence being much higher in low-income, African American neighborhoods of Detroit, Atlanta, Chicago, and Philadelphia, where violent crime rates are high. PTSD is linked to a broad range of negative consequences, including increased morbidity and mortality rates and higher risk for suicidal behavior. By way of example, one study showed that the mortality rate among Vietnam veterans with PTSD was 71 percent higher than veterans without PTSD. Such increased mortality was primarily explained by suicide and motor vehicle accidents. A recent study showed that soldiers who suffered from PTSD were 5.4 times likelier to experience suicidal ideation. In addition to this, the likelihood of suicidal ideation was 7.5 times higher among soldiers with at least two comorbid conditions than among those with PTSD only. Although only a minority of those exposed to TEs develop PTSD, many who do not meet full criteria may nonetheless be classified as experiencing sub-threshold PTSD, with symptoms that are often clinically significant but treatable. There is a broad range of psychological consequences of TEs, including depression.
It is worth noting that diagnosable mental illness is only the “tip of the iceberg” in terms of the behavioral consequences of TEs. Common physical and behavioral responses—including nausea; dizziness; changes in sleep and appetite; withdrawal from daily activities; and feelings of fear, grief, and depression—are much more frequently experienced. Although such responses can last for weeks or months, most people report feeling better within three months after a TE. It is only a minority of persons who proceed to, or continue to experience, diagnosable pathology (Figure 2).
Figure 2. Mental health consequences of traumatic event experiences
It is important to also note that TEs and their consequences are not confined to soldiers, or to persons who we may typically think of as being “in harm’s way.” I illustrate this by drawing on two studies in which I have long been involved. The Detroit Neighborhood Health Study examined lifetime experience of TEs and PTSD among predominantly African American residents of Detroit. Results showed that the lifetime prevalence of exposure to at least one TE was 87.2 percent, with the unexpected death of a loved one being the most prevalent single exposure, at 70.6 percent. The lifetime prevalence of PTSD in this sample is 17.1 percent, and is most common among people who experienced assaultive violence, especially among those who have been raped (32.8 percent) or been badly beaten (31.2 percent). Strikingly, in a sample of Ohio Army National Guard soldiers, 77.6 percent experienced at least one TE in their most recent deployment, while the prevalence of deployment-related PTSD was only 9.6 percent—about half that estimated in the Detroit Neighborhood Study.
How Our Social, Economic, and Cultural Context Modifies the Effect of Traumatic Events
The ubiquity and breadth of the health consequences of TEs readily argue for their importance to the health of populations. Equally salient, however, is the interplay between TEs and the social, economic, and cultural context that shapes population health—the core remit of public health. TEs such as violence and war can rest on cultural conflicts that have motivated human made mass traumatic events, forces that are powerful and are unfortunately encouraged by contemporary turmoil. But the contextual drivers of the consequences of TEs can be much more quotidian. For example, supportive networks and social support at the neighborhood level have demonstrated salutary effects on mental health. Collective efficacy, which is defined as “social cohesion among neighbors” and their willingness to intervene for common goods, has been found to help reduce physiological distress and the risk of mental health disorder among residents who experienced loss of resources caused by natural disasters. Collective efficacy can function as a coping resource or mechanism and can have a positive impact on mental health through its link with other neighborhood indicators like poverty or crime. For example, a study of those exposed to the Florida 2004 hurricanes found that collective efficacy was linked with a decreased likelihood of PTSD and depression symptoms. A study of people exposed to Hurricane Sandy showed that higher levels of perceived neighborhood social cohesion, which is a component of collective efficacy, are strongly linked with decreased levels of PTSD symptoms (Figure 3). Examining interactions between individual and community-level factors after Hurricane Sandy, our group found that people with more disaster-related stressors (e.g. displacement, property damage) and who lived in communities with more damage tended to have higher individual service need.
Figure 3. Moderating effect of neighborhood social cohesion on the impact of exposure on symptoms of post-traumatic stress
Heid AR, Pruchno R, Cartwright FP, Wilson-Genderson M. Exposure to Hurricane Sandy, neighborhood collective efficacy, and post-traumatic stress symptoms in older adults. Aging and Mental Health. 21(7): 742—750.
The Societal Cost of Traumatic Events
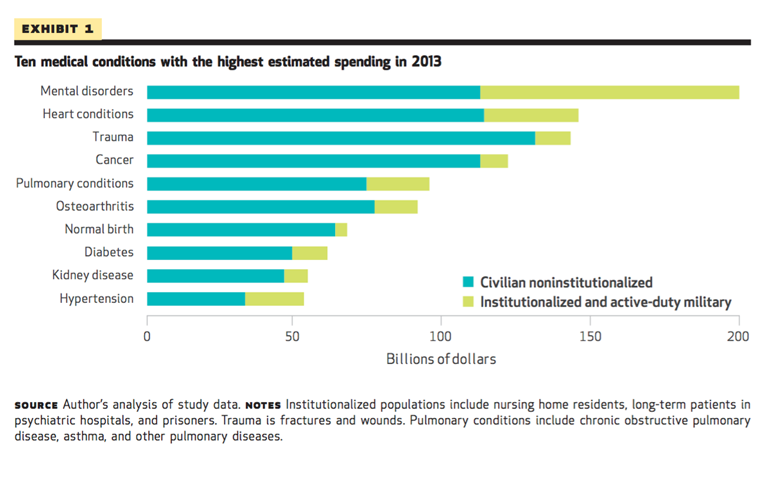
Beyond the burdens that TEs impose on individuals and families, TEs also account for a huge financial cost to society. In 2013, trauma was among the top three medical conditions with the highest estimated spending (Figure 4). Mental disorders were the costliest disorders, with many of these cases also linked to TE experiences.
Figure 4. Ten medical conditions with the highest estimated spending in 2013
Roehrig C. Mental Disorders Top The List Of The Most Costly Conditions In The United States: $201 Billion. Health Affairs. 2016; 35(6): 1130—1135.
Among those who experience TEs, those with PTSD have among the highest rates of healthcare service use. A Congressional Budget Office report pointed out that veterans suffering from PTSD are more likely to require longer periods of treatment because their clinical conditions may be more complicated and take longer to resolve. In addition, those patients need more intensive initial use of services, which may predispose them to seek continuing care. Between 2004 and 2009, the Veterans Health Administration (VHA) spent more than half its funding on post-9/11 service members with PTSD and/or TBI. The Congressional Budget Office (CBO) estimates that during the same time period, the VHA spent $2.2 billion on patients with PTSD, TBI, or both. A full accounting of the costs of TEs domestically and globally must also include the cost to society in terms of non-healthcare costs such as lost wages and productivity, and time spent disabled, a figure that would undoubtedly eclipse the best available estimates.
In Summary
I have often felt that TEs represent a little-discussed, dramatically important determinant of the health of populations. While the Thai soccer team’s ordeal represents a particularly dramatic example of trauma, TEs are, in fact, remarkably common, and have important health consequences for billions worldwide. Importantly, these consequences can be mitigated substantially through investments in the social, economic, and cultural context within which we live, mitigating both the traumatic event itself and its consequences.
I hope everyone has a terrific week. Until next week.
Warm regards,
Sandro
Acknowledgement: I am grateful to Gregory Cohen, MPhil, MSW, and Shui Yu, MA, for their contributions to this Dean’s Note.
Previous Dean’s Notes are archived at: http://www.bu.edu/sph/tag/deans-note/